Shoulder Pyrocarbon Hemiarthroplasty
Pyrocarbon hemiarthoplasty is an alternative shoulder replacement for young patients or patients with high physical demands. There have been 2 pyrocarbon hemiarthoplasty implants produced.
 Tornier Wright
Tornier Wright Pyrotitan Resurfacing Implant
Pyrotitan Resurfacing Implant
Hemiarthroplasty is where only half of the joint is replaced. In shoulder hemiarthroplasty the humeral (ball) side is replaced. Shoulder hemiarthroplasty was invented for fractures and later adapted for use in shoulder arthritis. The humeral head was replaced at surgery with a metal (chrome cobalt) head. However, the metal heads could erode the native socket (glenoid), causing pain and the need for revision surgery. To resist this painful wear, plastic (polyethylene) sockets were cemented into the glenoid. In younger or high demand patients there is concern regarding the longevity of the plastic socket and bone loss due to inflammation from plastic wear particles.
Why Pyrocarbon?
Pyrocarbon has material properties suited to hemiarthroplasty. Pyrocarbon is a synthetic compound, produced at extreme temperatures and coated onto graphite.

Pyrocarbon has strength and wear properties between those of graphite and diamond. It is biocompatible, having been used in cardiac valves for more than 30 years. It has been used to replace joints in the hand and elbow. Pyrocarbon has similar mechanical properties (modulus of elasticity) to cortical bone. Pyrocarbon demonstrates up to 300 times less wear on bone than zirconia and medical grade metals.
Indications for Pyrocarbon hemiarthroplasty include:
- humeral head collapse (avascular necrosis)
- Osteoarthritis
- Secondary arthritis.
- Fractures that damage the humeral articular surface
Historical use of Pyrocarbon Shoulder Hemiarthroplasty
The first use of a stemmed Pyrocarbon shoulder hemiathroplasty in Australia was in 2014.
There has been 1 publication “Pyrolytic carbon humeral head in hemi-shoulder arthroplasty: preliminary results at 2-year follow-up” ( Garret et al, JSES, Vol3, Issue1, P37-42, March 01,2019).
In the Australian Orthopaedic Association National Joint Replacement Registry 2019, the Pyrotitan pyrocarbon resurfacing hemiarthroplasty had the best survival of primary hemi resurfacing shoulder replacement for osteoarthritis.
My Experience with Pyrocarbon Hemiarthroplasty
I have used the Tornier-Wright stemmed pyrocarbon hemiarthroplasty (examples above) on greater than 25 occasions from 2014-20 and continue to use the prosthesis. The surgery is performed with general anaesthesia and arm block. The surgery takes 90 mins - 3 hrs depending on complexity. Most patients are discharged home after a 1-2 nights stay in hospital. Patients note after the surgery the chronic deep-seated arthritic pain has improved. The pain from the surgical procedure settles over several days. Initial post-operative pain killers are usually opiate based and can cause constipation. A high fibre diet and additives (Coloxyl, Movicol) are encouraged. Transfer to a rehabilitation hospital is not required. The wound is covered with a waterproof dressing that allows showering the day after surgery. The dressing should remain intact until the 2 weeks review. Bruising can be seen extending down the arm and this is normal. A sling is required for 6 weeks after surgery to allow the front tendon to reattach. Driving can be gradually restored after sling removal and ceasing pain medication. Patients are instructed in a stretching program that can be self-directed. Formal physiotherapy is normally commenced around 6-10 weeks post- surgery.
Risks of the surgery, specific to the procedure are low but include infection, stiffness, nerve and vascular injury, fracture and dislocation. General risks related to surgery and anaesthesia, such as stroke and heart attack are rare. A pre-operative review by any treating specialist (eg. Cardiologists) is recommended. The longevity of the implant has not been accurately defined due to its recent introduction.
Preparation for Surgery
Things to consider:
- A CT scan is obtained prior to surgery to assist with computer based modelling of sizes.
- If the surgery is on your dominant arm; practicing tasks with your other arm in the weeks leading up to surgery will assist with independence in activities of daily living.
- Meals can be prepared prior to surgery to minimise cooking loads in post-operative period.
- Sleeping can be difficult in a sling after surgery. Some patients find it easier to sleep in a recliner, that can be hired. Extra pillows can be used to pack around the arm.
- Risk for infection can be further reduced prior to surgery by showering and washing the shoulder with Benzac AC 5 % wash for 3 days prior to the surgery.
Rehabilitation
After the surgery you will be placed in a sling.
From the first day after surgery you will commence shoulder and elbow range of motion exercises.
Stage 1 (0-6 weeks)
Repeat each exercise 10 times. Do 3 sessions per day.
Passive Shoulder Elevation 1: With the help of someone, relax your arm completely while they slowly lift your arm as comfortable and lower it again. You should be aiming to get to 90 degrees to your body unless told otherwise.

Passive Shoulder Elevation 2:
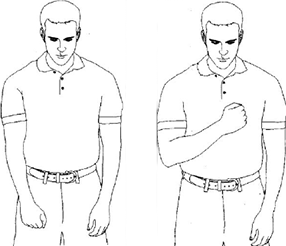
Relax with your arm across your chest supported by your other arm. Slowly lift your arm as comfortable and lower it again.
You should be aiming to get to 90 degrees to your body unless told otherwise.

Passive Shoulder Elevation 3:
In either sitting or standing, support your operated are with your other arm. Lean forward to allow gravity to assist you to lift your arm as comfortable and lower it again.
You should be aiming to get to 90 degrees to your body unless told otherwise.

Shoulder External Rotation:
Relax your arm completely with your hand resting on your stomach. Keep your elbow by your side and with the help of your other arm rotate your hand from your stomach so that it is pointing out from your body.
Relax as you return your arm to rest on your stomach.

Elbow bending/straightening: With your arm resting on your stomach, slowly straighten your elbow as far as you can, then bend your elbow again. Keep the palm of your hand facing your body. You may be instructed to do this exercise with the assistance of the other hand depending on what type of surgery you have had.
Wrist and Finger Movements:
1. Move your wrist forwards and backwards and from side to side.
2. Make a fist with your fingers and then stretch them out as far as you can.

Stage 2 (6-12 weeks)
After the sling is removed a gentle stretching program can commence. No weights or resistance bands are used until 12 weeks post-surgery.
Stage 3 (12 weeks +)
Exercise 1Flexion:Using theraband, start with your arm at your side and pull forward. Keep your elbow straight.

Exercise 2Extension:Using theraband, pull your arm back. Be sure to keep your elbow straight.

Exercise 3Adduction:Using theraband, pull your arm toward your side. Keep your elbow straight. Do not twist or rotate your trunk.

Exercise 4Abduction:Using theraband, keep your elbow straight and pull from your body out to the side as shown.

Exercise 5External Rotation:Using theraband keep your elbow at your side and rotate out to the side.

Exercise 6Internal Rotation:Using theraband keep your elbow at your side and rotate in toward your body.

Return to activities:
Breaststroke swimming and light resistance exercises can commence around 12 weeks post-surgery. Lifting can increase by 1 kg per fortnight from 12 weeks guided by pain. Return to physical work or fitness will take 4-6 months. Impact sports such as boxing are best avoided long term.